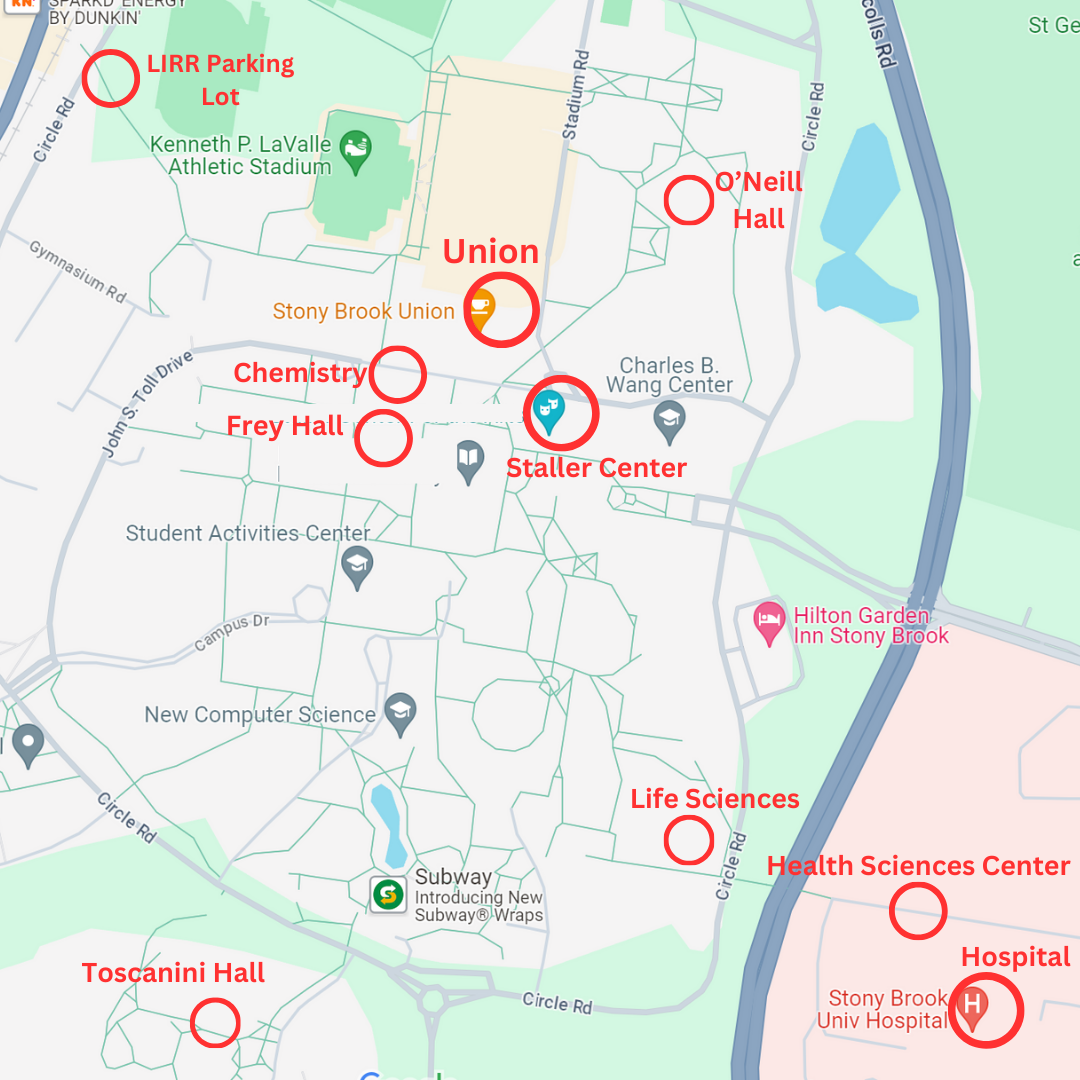
A team of researchers at Stony Brook University conducted a pilot study that suggests there may be a link between chronic post-traumatic stress disorder (PTSD) in 9/11 responders and cognitive degeneration, leading to diseases like Alzheimer’s.
Thousands of first responders and survivors from Ground Zero are still coping with 9/11-related illnesses such as PTSD. Organizations like the World Trade Center (WTC) Health Program and the Stony Brook WTC Wellness Program that conducted the study provides health support and medical treatment for first responders who are in need of care.
The study’s sample included 34 first responders, half of whom identified as having symptoms of PTSD such as re-experiencing stressful memories that induce physiological distress. Blood samples from the responders were collected to analyze the concentrations of three biomarkers that are measures of neurodegeneration: beta-amyloid, tau and neurofilament light.
“What makes [this study] unique is that responders are followed for every year to every 18 months since 2002, so we know a lot about their PTSD,” Sean Clouston, an assistant professor in the Department of Family, Population and Preventive Medicine and the study’s lead researcher, said.
Before conducting the study, Clouston theorized that people with PTSD are at a greater risk of experiencing early aging. After monitoring patients at the WTC Wellness Program, Clouston and his team of researchers found that PTSD was associated with cognitive impairment affecting memory functions, physical functioning and the brain’s ability to process information.
The study found that higher levels of the beta-amyloid marker — a type of protein that builds up in the brains of Alzheimer’s patients — was highly correlated with PTSD.
Benjamin Luft, director of the WTC Wellness Program, said that his organization was initially established as a voluntary clinic to serve Long Island’s first responders who did not have health insurance after 9/11.
“We began the program in what we call a ‘collaborative way’ between doctors, nurses, social workers and other psychologists where they’re very sensitive to not only a variety of medical conditions but also the psychological and social problems that people may have,” Luft said.
Referring to the study, he said that “it is part of a puzzle that we’ve been working on for many years.”
“[The program’s] collaboration and integration between specialties show that even though things may predominantly manifest themselves psychologically, they have a tremendous amount of physical effects,” Luft said.
Luft emphasized that the responders’ physical, psychological and psychiatric health are intertwined and need to be treated equally. The program and the study sheds light on how traumatic exposures like 9/11 impact long-term human suffering
By identifying a biomarker for PTSD and the patients’ cognitive problems, the responders get a sense of their own risks of experiencing neurodegenerative diseases. This is important, according to Clouston, because one of the problems with neurodegenerative conditions is that there is not a way to regrow brain material after neuron cells die; any medical intervention has to be done early in the process when patients start to experience aging.
Determining these risks allows medical experts to check what might be worth measuring and double-checking for patients who are suffering from chronic PTSD for more than a decade after their traumatic exposures.
“One of the reasons why I actually do this work is that I’m interested in understanding this foundational problem in the social sphere, which is this long-standing problem — exposures in midlife appear to affect your lifelong trajectories,” Clouston said.
John Feal, a 9/11 first responder, is the founder of the FealGood Foundation, an organization that works to inform elected officials and private entities of the concerns and illnesses faced by first responders. During the recovery mission, his left foot was mangled under steel wreckage. After several surgeries and a PTSD diagnosis, Feal steered his suffering and vulnerability toward a larger goal that speaks to his foundation’s motto: “No Responders Left Behind.”
“I didn’t have the FealGood organization to advocate for me,” Feal said. “I had to fight for myself.” Feal’s organization depends on grassroots activism to advocate for the care of first responders who have been denied compensation for their sacrifices.
The foundation’s small beginnings, collecting donations and selling t-shirts, led up to one of Feal’s greatest accomplishments: the passing of James Zadroga 9/11 Health and Compensation Act in 2010. When the law passed, it provided health monitoring for first responders and survivors as well as funding for the WTC Program.
Institutions like the Stony Brook WTC Wellness Program, “have the responsibility to not only treat us but use us as data,” Feal said. “9/11 will be used as a model. It’s vital that they continue to research the after-effects of those affected by 9/11 and their post-traumatic.”
Clouston and his team plan on expanding their research by enlarging the sample size and factoring in more biomarkers that can potentially further support the study’s findings. Two influential additions to their research include looking into neuroimaging studies and changes in the immune system.
By looking at magnetic resonance imaging (MRI) scans, researchers will be able to detect neurodegeneration in the brain. Also, Clouston said that when “experiencing chronic stress, [the brain] dysregulates the immune system,” so the new study will explore changes in the neuroimmune system and broaden the blood marker spectrum to strengthen the link between PTSD in first responders and cognitive diseases.
“Working with first responders gives you a sense of the tremendous amount of sacrifice that patients or people do,” Luft said. “When people act heroically we are thankful, but we don’t realize that when people are doing those things, they are losing something.”