Ranomafana, Madagascar – On Aug. 23, 2017, a 31-year-old Malagasy man began experiencing malaria-like symptoms while in Ankazobe District, Madagascar. Over the next few days he planned to travel across the central plateau to his home in Toamasina. He traveled by taxi brousse, an often overcrowded minibus and the country’s most common form of transportation. This route took him through the capital city of Antananarivo, where he had to spend time in a transportation hub while waiting to switch to a new taxi brousse. On Aug. 27, he died on that taxi brousse shortly before arriving in Toamasina.
Three weeks later, on Sept. 11, a 47-year-old woman who traveled in one of the taxi brousses with the initial victim, was admitted to and later died at Soavinandriana Hospital Center in Antananarivo. She, along with everyone else who was in a taxi brousse with the first victim, was diagnosed with pneumonic plague.
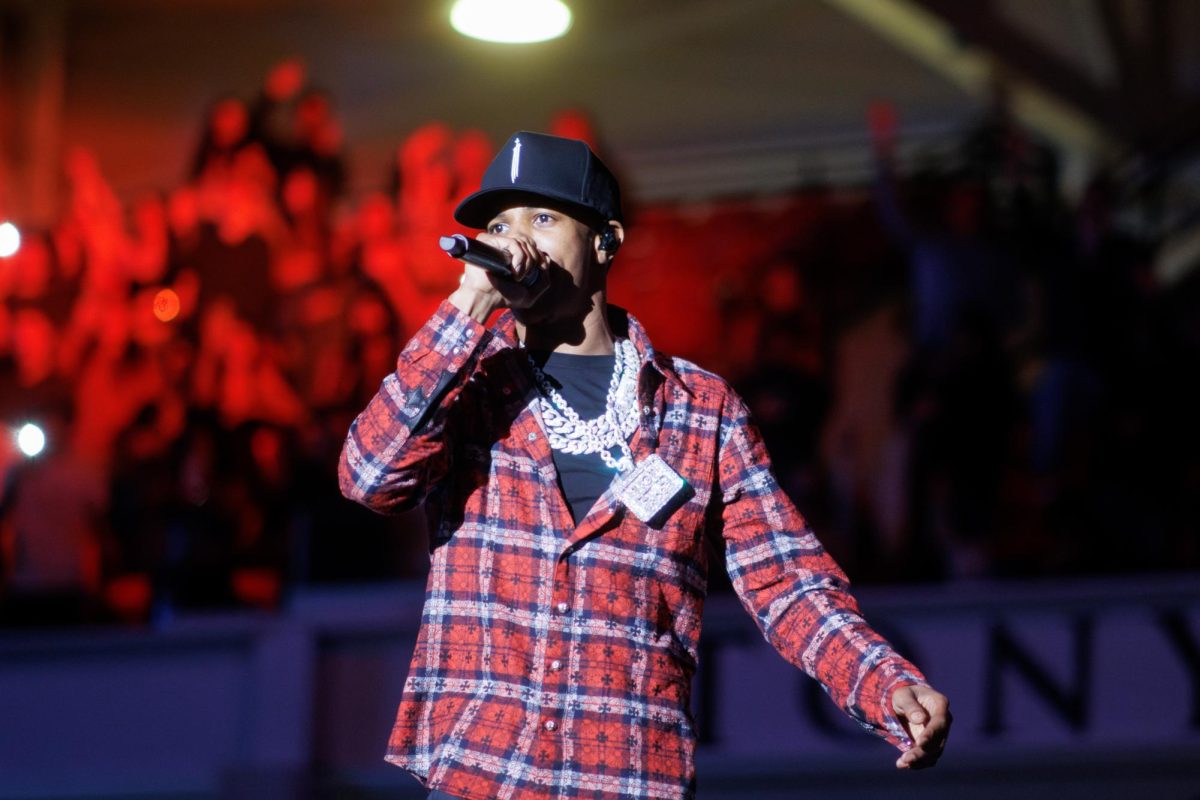
There are currently 17 Stony Brook University students studying abroad at Centre ValBio in Ranomafana, Madagascar. While some of the study abroad activities have been altered to limit contact with the disease, the university is confident about their safety. Alicia Lamb, the teaching assistant on the trip, said, “I think that the precautions that the university has taken are extreme but understandable. I am not worried about my health or the health of the students at all. In the unlikely chance that one of the students were to contract the plague, it is very treatable and the medication is readily available to us.”
Plague is an infectious disease caused by the bacteria Yersinia pestis. There are three forms of the plague: bubonic, pneumonic and septicemic, that are differentiated based on where in the body the infection occurs. Bubonic plague infects the lymphatic system, pneumonic plague infects the lungs, septicemic plague infects the bloodstream.
Bubonic plague is the most common form of the disease, transmitted through flea bites. Pneumonic is the deadliest form, transmitted from person to person through bacteria infected droplets. “Pneumonic plague in an urban environment can spread rapidly and that’s really where they got unlucky this year,” Dr. Peter Small, the founding director of Stony Brook University’s Global Health Institute (GHI), said. Without treatment, individuals who contract pneumonic plague have almost a 100 percent mortality rate.
As of Nov. 6, the World Health Organization (WHO) identified 364 confirmed cases of plague in Madagascar and the Ministry of Public Health had reported 143 deaths.
A major dilemma facing health care providers in areas outside of Antananarivo is a lack of access to rapid diagnostic tests. “Confirming a case of plague is an arduous process that requires either culture of the highly pathogenic bacteria or a combination of other laboratory assays,” said Dr. Simon Grandjean Lapierre, an infectious disease specialist who works for the GHI in Madagascar. “Tests that, due to biosecurity considerations, can only be performed in the Institute Pasteur of Madagascar, a WHO plague reference laboratory. In this context, community health workers and other healthcare personnel adequately diagnosing, empirically treating cases and tracing contacts in remote areas of the country are essential for adequate outbreak control.”
In response to the outbreak, the Ministry of Public Health has stationed doctors and nurses at police road stops around the country to assess the health of individuals traveling in taxi brousses and other automobiles from affected areas. The ministry has also mobilized thousands of community health workers and hundreds of doctors and medical students to trace the path of this outbreak and to perform active case finding.
“With a response that focused heavily on awareness raising and contact tracing, the government and its partners achieved a decline in the incidence of pneumonic plague after the peak of the outbreak in mid-October,” said Dr. Astrid Knoblauch, an epidemiologist at the Institute Pasteur of Madagascar. “However, each case of pneumonic plague could potentially start a new upsurge of cases.”
The government has also asked people to not participate in the Famadihana ceremony, a tradition in some parts of Madagascar known as “the turning of the bones.” In this ceremony, people disinter and unwrap the remains of their deceased family members and dance with them, sometimes for multiple days, before rewrapping the remains and entombing them. Some news outlets have inaccurately reported that the ceremony has contributed to this year’s outbreak. However, it is possible that disinterring individuals who have died during this outbreak will infect participants in future years.
Connor Johnson, a Peace Corps health volunteer from the Toamasina area, said that despite the government’s warning about the health risks, he witnessed a Famadihana ceremony last week. “Life hasn’t been all that different since the outbreak,” he said. “People are justifiably scared but haven’t altered their day-to-day life, it’s just another topic to talk about while having coffee or a beer.”
For many people in the western world, the word “plague” conjures up images of the historical outbreaks that occurred in Europe in the 14th century, killing an estimated 50 million people. In a conversation about the plague outbreak, Dr. Small explained that “there’s nothing surprising about diseases of antiquity killing people who live in poverty.”
In some places, health care systems and living conditions have advanced far beyond what they were in 14th century Europe. However, in places like Madagascar, they unfortunately have not. “Madagascar is one of the poorest countries in the world and despite their best efforts they simply don’t have the public health system that we have in richer countries and so when you have a bacterium that is endemic it becomes a lot more difficult to control,” said Dr. Small.
According to the Ministry of Public Health, there are approximately 400 cases of bubonic plague recorded each plague season that lasts from August to April. Most of these cases occur in small, remote villages far away from major population centers, leaving little room for an outbreak to occur. The WHO defines an outbreak as, “an occurrence of cases of disease in excess of what would normally be expected in a defined community, geographical area or season.”
The WHO has issued a level 2 travel alert for Madagascar, the same level of travel alert that they have issued for Zika virus-affected countries. It recommends that anyone traveling to the country “practice enhanced precautions” and has deemed the international risk “low” because Madagascar is an island nation, the international mobility of the affected population is low and the incubation period of pneumonic plague is very short. They have advised travelers not to restrict any travel to the country and have expressed confidence in the safety of tourism.
Plague is endemic to numerous places around the world including the United States. According to the Centers for Disease Control and Prevention, there are on average seven cases of plague in the U.S. each year; over 80 percent of those cases have been the bubonic form of the disease.
“Be careful though,” Dr. Small warned, “before the United States gets too smug about the situation, we should remember that the only difference between a plague case and a plague epidemic is a good public health system and ours is being eroded by the current federal government’s budget cuts.”