Anat Biegon, a professor in the department of radiology at the Renaissance School of Medicine, co-wrote a study that found taking sex into account could change diagnoses for 20% of people with Mild Cognitive Impairment (MCI).
The study looked at verbal memory tests, which are early indicators of MCIs like dementia. The tests measure how many words someone can remember after a period of time. Women tend to do better on memory tests, but this advantage may mean a misdiagnosis when it comes to cognitive impairments. Biegon said that because women score higher on these tests, they don’t receive their diagnosis as quickly as men. Often times, they get it later down the line.
Women often don’t get a diagnosis until later because they don’t display symptoms such as mood changes and confusion that constitutes as Alzheimer’s, as quickly as men do, even if both show the same signs in the brain indicating the disease.
“They have to go further down before they will be diagnosed or recognized as actually having an impairment,” she said. “We figured this could be the reason because they have a cognitive reserve. They start from a higher point.”
The study found that when these tests were evaluated on sex rather than average scores, 10% more women were diagnosed with MCI and 10% of men were undiagnosed.
The study had 985 participants from the Alzheimer’s Disease Neuroimaging Initiative. Participants were given 15 words with no correlation to each other and asked to repeat them back immediately. They were asked to recall those words again 20 minutes later.
“People with Alzheimer’s disease, many of them can not remember any words 20 minutes after exposure. Healthy people can remember 10 to 12,” Biegon said.
One indicator of Alzheimer’s is the deposition of amyloid — an abnormal protein that acts as a signal for some diseases — on the brain.
“By the time overt symptoms of Alzheimer’s occur, the amyloid is already up there,” she said. “The increased levels of this protein in the brain, they begin to increase 10 to 20 years before the person actually has symptoms.”
Michelle M. Mielke, professor of neurology and epidemiology, was also involved in the study. Mielke works at the Mayo Clinic, a medical center focusing on clinical research and scientific practices, where she specializes in neurological diseases and sex-specific differences.
“It’s possible that it is taking women longer to be diagnosed,” Mielke said. “Sex-specific norms are important cases in verbal memory.”
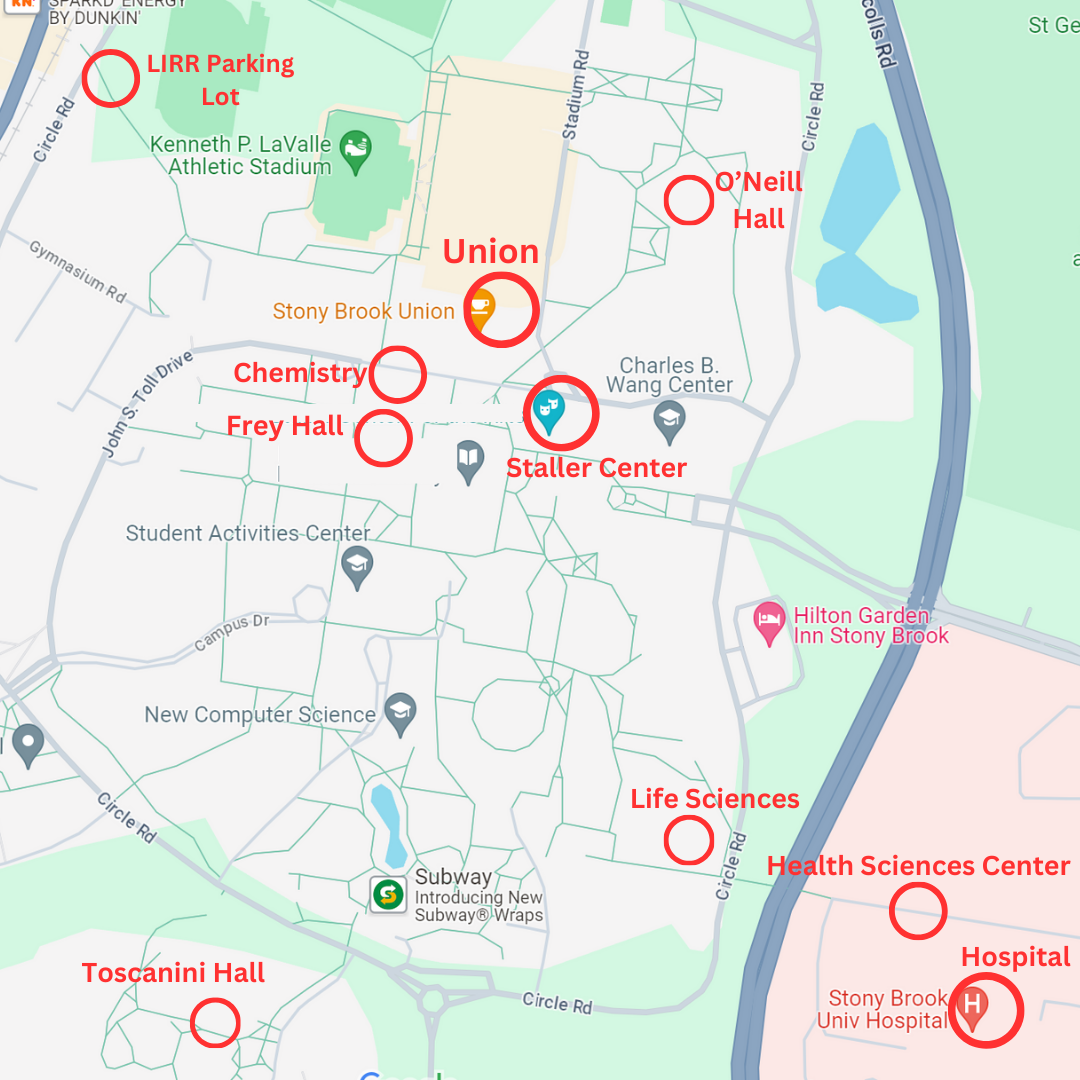
Christopher Christodoulou, a neuropsychologist in the Center of Excellence for Alzheimer’s Disease at Stony Brook Neurosciences Institute, said that neuroscience studies typically don’t take sex into account.
“A lot of studies, drugs for instance, have not been tested on women,” he said. “The push is to include all folks eligible and willing.”
The study has also prompted further research that will focus on sex differences, according to Biegon.
“We suspect that not only the verbal memory part of Alzheimer diagnosis needs to be made sex-specific; the whole diagnostic needs to be sex-specific,” she said.
Biegon added that follow-up research will aim to identify if future studies should adjust diagnosis tools, such as screenings and scales, to be sex-specific as well.
Mielke said that they plan to take different approaches for further research, including looking at the role of sex-specific scoring in different ethnic groups.
“Going forward, we’ll establish better normative data for all new neurophysiology tests,” Mielke said.
Highlighting these disparities between men and women for MCI, according to Christodoulou, can be somewhat of an eye-opener.
“[It] should make people more sensitive to changes in cognition,” he said.
Biegon, who said she’s seen misdiagnoses firsthand, wants to ensure that the proper measures are being taken to avoid any mistakes in people’s treatments.
“Being told you have Alzheimer’s [when] you don’t can be a burden,” she said. “Alzheimer’s steals your soul. You’re no longer you. You are your memories.”