Death lurks in first kisses, in almond butter jars and in movie theatre popcorn for 18-year-old Kristen Pittaro, a freshman psychology major at Stony Brook University.
Allergies are not limited to the kitchen. They follow her around to makeup stores, restaurants and outings with her boyfriend. They push her grocery and hospital bills exceptionally high. They feast on her mental health and are a source of her anxiety. As an adolescent, she recalls panicking over “that first kiss moment, being almost there and then thinking, wait, what did you eat today?”
Food allergies in children have skyrocketed 50% between 1997 and 2011, according to the Centers for Disease Control & Prevention. Roughly two children in every classroom have food allergies and a third of those children are bullied as a result, according to statistics collected by Food Allergy Research & Education.
Other than sapping time and money, food allergies take a “psychological toll” because of the constant struggle to fit in, Dr. Lorraine Danowski, a clinical nutrition instructor at Stony Brook University Hospital said.
As a child, Pittaro intentionally did not attend birthday parties to avoid having a potential allergic reaction. As a teenager, she has been left out of ice cream parlor hang-outs and date nights at Chick-fil-A.
From the health-conscious community, a person is frowned upon if they choose cow’s milk over macadamia nut milk. But for Pittaro, walking into her local health food store is a dance with death. Kevin Hall, a researcher at the National Institutes of Health, says that nearly all diets agree that people should avoid ultra processed food. Generally-speaking, that means if a person can’t pronounce it, they should not eat it. But the healthy-living food mantra does not apply to Pittaro.
“If I can’t pronounce it,” she says, “it’s more than likely safe.”
These safety measures are expensive. For the average American child, food allergies cost $4,184 each year for expenses including medicine, safe foods and loss of work, according to the National Library of Medicine. For the Pittaro family, one six-hour emergency room visit can cost $1,800 — and that’s including insurance.
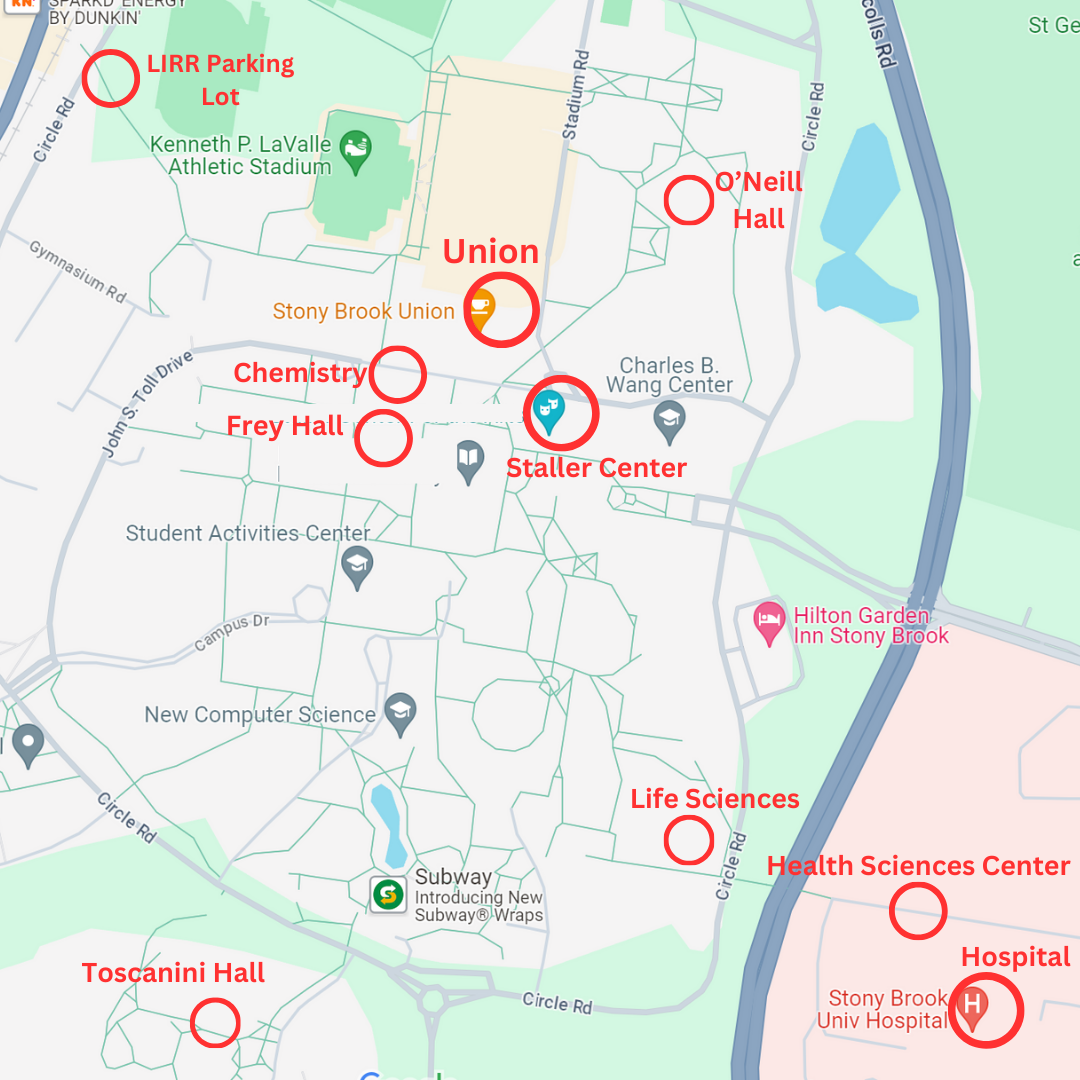
Accessing safe foods for Pittaro translates to leaving her dorm at Stony Brook University each week to drive home, a 45-minute round trip, and prepare meals in bulk for the upcoming week. Still, her mother Ann Pittaro remains on edge because she is unable to fully supervise her daughter’s food intake. If Kristen makes one slip, she can end up in the emergency room.
Anything can be a death trap: a seemingly harmless lollipop, mascara or hand sanitizer are among the possible dangers. “It’s just a lollipop,” Ann Pittaro said. “But you don’t know where it was made.”
Although she doesn’t have airborne allergies, Pittaro’s reactions are not purely autoimmune; just knowing the potential danger in her surroundings can give her anxiety. “If there’s enough in the air, I start to get a headache,” she said.
Even shopping at Sephora, the makeup paradise, is a grueling process for Pittaro. Shea butter, a fat extracted from the nut of the African shea tree, is a common ingredient to creams, soaps, lotions, hair products and makeup — which means they are forbidden for Pittaro. Shea butter is currently a top 20 ingredient in new cosmetic launches, according to Beauty Packaging.
Shellfish, peanuts, tree nuts and cellulose are a few of Pittaro’s many allergens. Fast-food chains like Chick-fil-A and Wendy’s are “absolute death traps,” Pittaro said. “Everything there is cross-contamination central.” But the list doesn’t end there. Restaurant desserts are off-limits and so is ice cream.
Before hanging out, Kristen’s boyfriend, Michael Rosenblatt, brushes his teeth “religiously” for two to three minutes, gargles with mouthwash, and flosses carefully. He keeps an “eye on her all the time,” but her allergies are “not a deal-breaker” in dating her, he says. “It’s who she is.”