After analyzing the data from 16 clinical trials, Stony Brook researchers confirmed earlier findings that a widely used cancer drug may be killing patients rather than saving their lives.
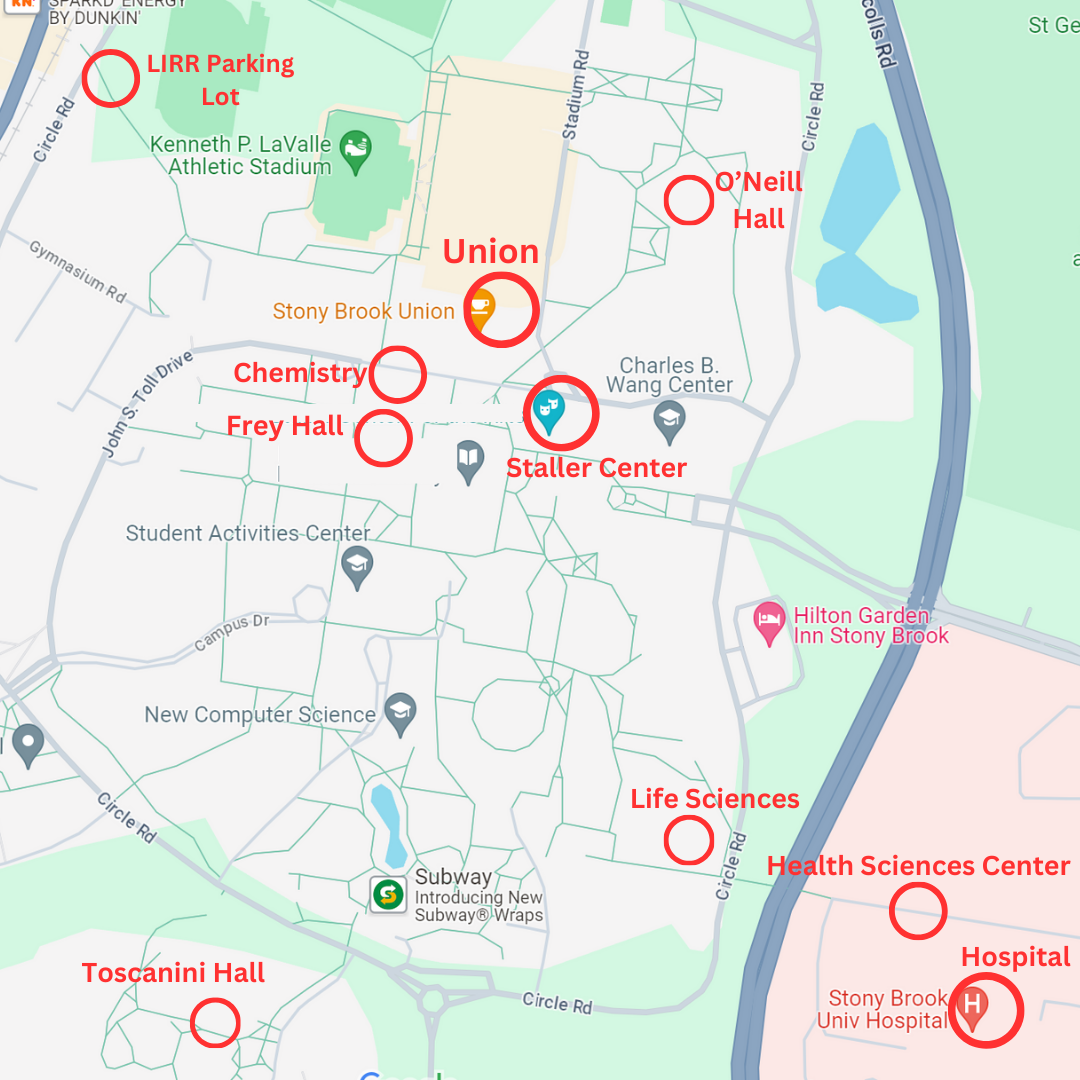
Marketed under the brand name Avastin, the drug was increasing treatment-related patient deaths by nearly half compared to patients taking only chemotherapy drugs, wrote the authors of a study published February in the Journal of the American Medical Association. Shenhong Wu, Sanjaykumar Hapani, and David Chu, researchers at the Stony Brook University Medical Center, conducted the study.
The intravenous solution was prescribed along with chemotherapy to combat metastasized breast cancer, as well as cancers of the lung, kidney, brain and colon. Its manufacturer, Genentech, claimed it stopped the growth of tumors by blocking the growth of blood vessels that provide tumors with nutrients.
Earlier studies showed Avastin was not effective against breast cancer and instead increased the likelihood of dangerous side effects in those patients. In December, the federal Food and Drug Administration removed breast cancer from the list of disease for which Avastin should be prescribed.
The Stony Brook team said it confirmed the most dangerous and common side effects were perforations of the intestines, heart, lungs, and nasal passages. Other blood disorders can also develop from the drug’s use, and patients who had recent surgery experienced more trouble healing.
Those side effects amounted to increased fatalities, already common in patients with cancer and other diseases where treatments are often extremely risky. To justify their use, oncologists must decide whether drugs like Avastin are more likely to prolong life than to take it.
Despite the known risk of intestinal perforation, many oncologists opted to prescribe the intravenous drug. But the new study’s conclusions may cause some to reconsider their prescriptions.
The Stony Brook analysis was the latest contribution to a growing controversy regarding the FDA’s accelerated approval system. While most new drugs must undergo several long-term clinical trials before being approved, the FDA makes exceptions for potentially lifesaving drugs used to treat deadly diseases such as cancer.
To more quickly get medicine to patients without long to live, drug companies may release their products temporarily after only one successful clinical trial. Then, two more clinical trials must be run if the product is to retain its approval.
In the case of Avastin, an accelerated approval allowed it to reach pharmacy shelves quickly. Even with the system in place, drug companies must conduct separate clinical trials for each disease they hope to treat.
So while Avastin has kept its approval for colon, kidney, brain, and lung cancers, four recent studies of its effects on breast cancer patients suggest that it does more harm than good.
A New Analysis
Wu said his duty to patients led him to re-examine such a successful drug. “Assessing side effects is very difficult but is also very necessary,” he said.
According to Wu, drug companies share this duty. Avastin’s maker publicly supported the team’s decision to further investigate Avastin.
“While negative publicity is not very good, the improvement of patient safety is extremely important,” said Wu.
Wu’s team first searched PubMed and other peer-reviewed journals for articles containing the words “Avastin,” “bevacizumab,” the generic compound name, and “cancer,” along with keywords relating to its potential side effects.
After finding over 300 potentially relevant articles, the team discarded all but 17 highly rigorous, randomized controlled trials the team identified as relevant and reliable. Among the 12,294 patients involved, a much higher mortality rate was observed among patients treated with Avastin.
While previous studies had documented Avastin’s side effects, this was not enough to determine its overall safety, according to Wu.
“Simply put,” he said, “the risk had not been quantified.”
With its statistical analysis, his team was able to see patterns where others had not.
The Future of Avastin
Dayna McCauley, a board-certified oncology pharmacist at the Stony Brook Medical Center, has personal experience dispensing Avastin and other high-risk cancer drugs. Pharmacists are required to re-take an eight-hour exam every seven years that tests their knowledge of drugs used in their specific field.
McCauley noted that chemotherapy drugs can be among the most dangerous.
“Drugs that are used to treat cancer patients tend to have a lot of side effects, which may include harm to the hospital workers that dispense them,” she said. “They are made in special pharmacies by people with training in how to make and handle them, and… their use is usually limited to attending physicians.
In her 25 years of oncology experience, McCauley said she has seen many new drugs emerge and understands the excitement that surrounded Avastin. She has observed that when clinical trials published before FDA approval are positive, oncologists are quick to begin using drugs once they are put on shelves.
For example, Taxol, a chemotherapy drug made from the bark of the Pacific yew tree, was shown to be extremely effective in combating ovarian and breast cancer. After being FDA approved, it was immediately adopted by many oncologists.
The same process held true for Avastin, according to McCauley. “The pre-approval clinical trials were extremely provocative and looked really good, because it’s the first drug that targets the molecule VEGF,” she said.
VEGF is a protein that delivers oxygen to tissue when blood circulation is cut off. By neutralizing it, Avastin can deny cancerous tumors the oxygen they use to grow and spread.
Another factor in determining drug adoption is the possibility of using one drug to treat many types of cancer. Some hospitals, like Stony Brook’s, allow drugs that have been approved to fight one type of cancer in experimental or “off-label” treatments for other cancers.
“Because we are an academic medical center, we allow off-label use if there is significant data to support a drug’s use,” McCauley said. Avastin began as an approved treatment for metastasized colon and rectal cancers, and was later approved for lung cancer, breast cancer, and others.
Currently, Avastin’s approval indication has so far been reassessed only for breast cancer. It is still deemed safe for other uses.
According to McCauley, 80 to 100 breast cancer patients were being treated at Stony Brook with Avastin. Now, however, some oncologists have begun to reevaluate their patients’ treatment plans, said McCauley.
The drug is still prescribed for those who were already responding to Avastin without serious side effects. Most oncologists, however, are not starting any new breast cancer patients on Avastin, said McCauley.
In terms of other cancers, Avastin has become what McCauley calls “the drug of the century.” Over 100 Stony Brook patients with a wide variety of cancers other than of the breast are being treated with it.
McCauley said that the main challenges for Avastin are occurring because it is the first drug of its class, designed to suppress VEGF. So far, most of its use has been restricted to patients with late-stage cancer and little hope for survival.
“But as they gain experience, [oncologists] will start using it in primary management – earlier and earlier in the treatment of diseases,” she said. “Right now, people are figuring out the best ways to use Avastin. I predict that it will be strong for years to come.”
Wu said he hopes that future studies will assist drug makers in decreasing Avastin’s risks. “It’s impossible to know how much difference [my team’s study] made at this point,” he said. “Our goal is to try to use this drug more safely.”