
Matt Venezia is a sophomore biology major with a minor in writing.
Over the course of the pandemic, I, like many others, have been tested for both SARS-CoV-2 antibodies and the presence of the virus itself. There is a lot of misinformation surrounding COVID-19, which extends to testing for the virus.
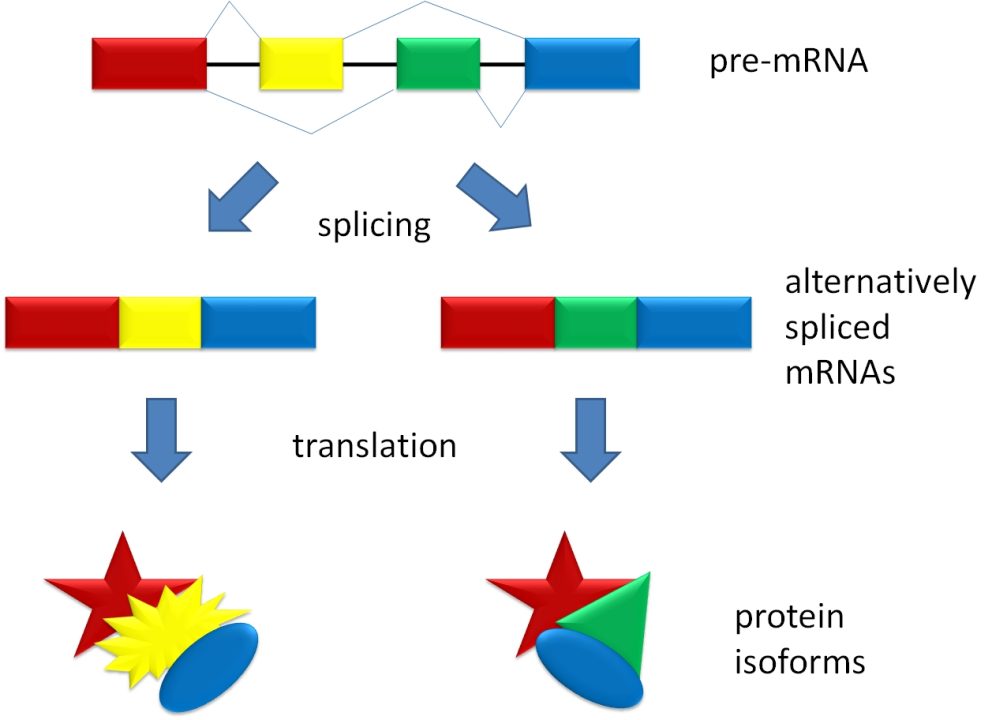
Currently, we rely on a process called reverse-transcriptase polymerase chain reaction (RT-PCR) to test for the presence of SARS-CoV-2, otherwise known as a diagnostic test. For this test, a nasal swab is taken from the person being tested. The swab is then sent to a laboratory, where RT-PCR is performed and the presence of the virus is either confirmed or denied.
Antibody tests are blood tests used to determine whether an individual has had exposure to the virus. They are not used to diagnose an infection with COVID-19. Antibodies are proteins created by the body in response to a pathogen, such as measles or SARS-CoV-2, in the bloodstream and are the only clinically significant indicator of previous infection.
New information about COVID-19 is being discovered rapidly and the facts surrounding testing are not well-established yet, so here are a few things to know before and after getting tested:
- False negatives for diagnostic RT-PCR tests are common early into exposure.
According to recent research, if you believe that you have been exposed to COVID-19, the best plan of action is to not get tested immediately. A new study suggests that false negatives are common within the first four days after infection, but after the fifth day, incidence of false negatives decrease rapidly from over 60% to under 30%. Another study found that from days one to seven of exposure, about 27% of nasal swab tests were falsely negative. In general, the reported rate of false negatives has ranged from 2% to 37% and is likely somewhere around 24%.
The possibility of a false negative should not dissuade anyone from getting tested, but this is a clear limitation of the RT-PCR test. Although the CDC recommends self-isolation for anyone experiencing COVID-19 symptoms regardless of a positive test, false negatives may make some asymptomatic carriers of the COVID-19 virus believe that they are not contagious, and as such have likely led to increased community transmission.
- False positives for diagnostic RT-PCR tests can happen, but they are rare.
False positives have also been reported to be a problem with RT-PCR tests. Though their incidence is rare, much more so than false negatives, false positives can occur. About 1% of RT-PCR tests result in a false positive, but some lab errors can also cause entire batches of tests to be falsely positive, as was seen in the National Football League in August. Despite this information, false positives do not seem to be a major issue with the RT-PCR test.
- The presence of antibodies does not necessarily mean you have immunity to COVID-19 permanently.
Currently, scientists do not know whether or not antibodies give permanent immunity to COVID-19. Scientists are also unaware if reinfection, or getting COVID-19 again, is possible. There is evidence which suggests antibodies remain in the body for months. Despite this, researchers cannot definitively say whether the presence of antibodies prevents reinfection with the virus. As a result, even if you are to test positive for COVID-19 antibodies, it is still imperative to treat COVID-19 as a potential threat and to follow CDC guidelines.
- Testing policy in the United States is still not where it should be, and access to rapid, effective testing depends largely on socioeconomic factors.
In America, results for an RT-PCR test usually come back within a few days, but this varies considerably depending on your location, your socioeconomic status and even your race. Many areas of the nation do not have access to rapid testing, meaning that tests may come back after a week or more. These areas are generally poorer, which means delivery services for essential supplies are not always available and households are more crowded, leaving patients in limbo unable to self isolate for the entire waiting period. Some who do not receive rapid testing are unwilling to self-isolate for the duration of the waiting period. These factors leave communities at risk of substantial transmission, some of which could be avoided with rapid testing. In fact, up to 40% of tests in the United States come back too late in order to effectively lead to a decrease in community transmission.
Testing policies are a complex issue. Current tests and testing policies are not perfect and there are limitations regarding the conclusions that we can draw from current research. There are likely to be some promising alternatives to the nasal swab RT-PCR test in the near future, such as saliva-based tests. With more time, a greater understanding will come of current and future tests along with their limitations. In time, research on the longevity of antibodies will also come along in greater quantities. With this, we will learn whether reinfection is possible or not. There is no telling if rapid testing will become available to the majority of Americans, but improvements are sure to come, as rapid testing is a major focal point of policy.
Right now, there is some uncertainty surrounding testing for COVID-19. Despite a lack of well-established facts, it is important to realize the necessity of being tested while also recognizing the drawbacks of current tests, so that you are able to get a clear understanding of what a negative or positive test result means for you specifically.
















Alice Carroll • Nov 3, 2020 at 3:34 am
It’s a relief to know that false positives are quite rare when it comes to COVID-19 testing. My roommate has been developing symptoms of it recently so I think she will need to self-quarantine a bit before getting tested. I guess it’s about time for my to start stocking up on more bottles of sanitary alcohol in order to disinfect more effectively.