Every other week Ruchi Shah, a biology major, will take a look at Stony Brook-related research and science news.
Cancer: a simple six-letter word that impacts the lives of millions. Yet, it is still an enigma to scientists. The complexity of the different types and subtypes of cancer makes the disease difficult to treat.
In addition, many of the chemotherapy drugs used today were developed decades ago and have limited effectiveness. Even if the drugs are effective, they often kill healthy cells as well, making it difficult for cancer patients to recover.
A research scientist in Stony Brook’s Department of Molecular Genetics & Microbiology by the name of Dr. Nobuhide Ueki is pioneering a technique to directly address the limitations of cancer treatment. He was further motivated to pursue this field of study after losing both of his grandparents to cancer.
His lab is focused on creating a drug delivery system that will selectively target cancer cells, leaving normal cells healthy.
In order to selectively target cancer cells, Ueki and his team began looking for markers such as proteins, enzymes or mutations that were expressed differently in cancer cells than in normal cells. Using a technique called an enzymatic assay, Ueki found that cancer cells have a higher level of the enzyme histone deacetylase, HDAC, when compared to normal cells.
Ueki used this enzymatic assay to compare levels of HDAC activity in normal cells and different types of cancer cells on a tissue culture plate. The same amount of a commercially available HDAC substrate was then added to each sample. The substrate specifically binds to the enzyme and releases a signal. The more enzyme present, the stronger the signal, which is quantified by a machine that measures the fluorescent light released in the signal.
Ueki found that all of the cancer types studied—including colon, pancreatic, cervical and breast cancer—had strong HDAC activity, while the normal cells did not.
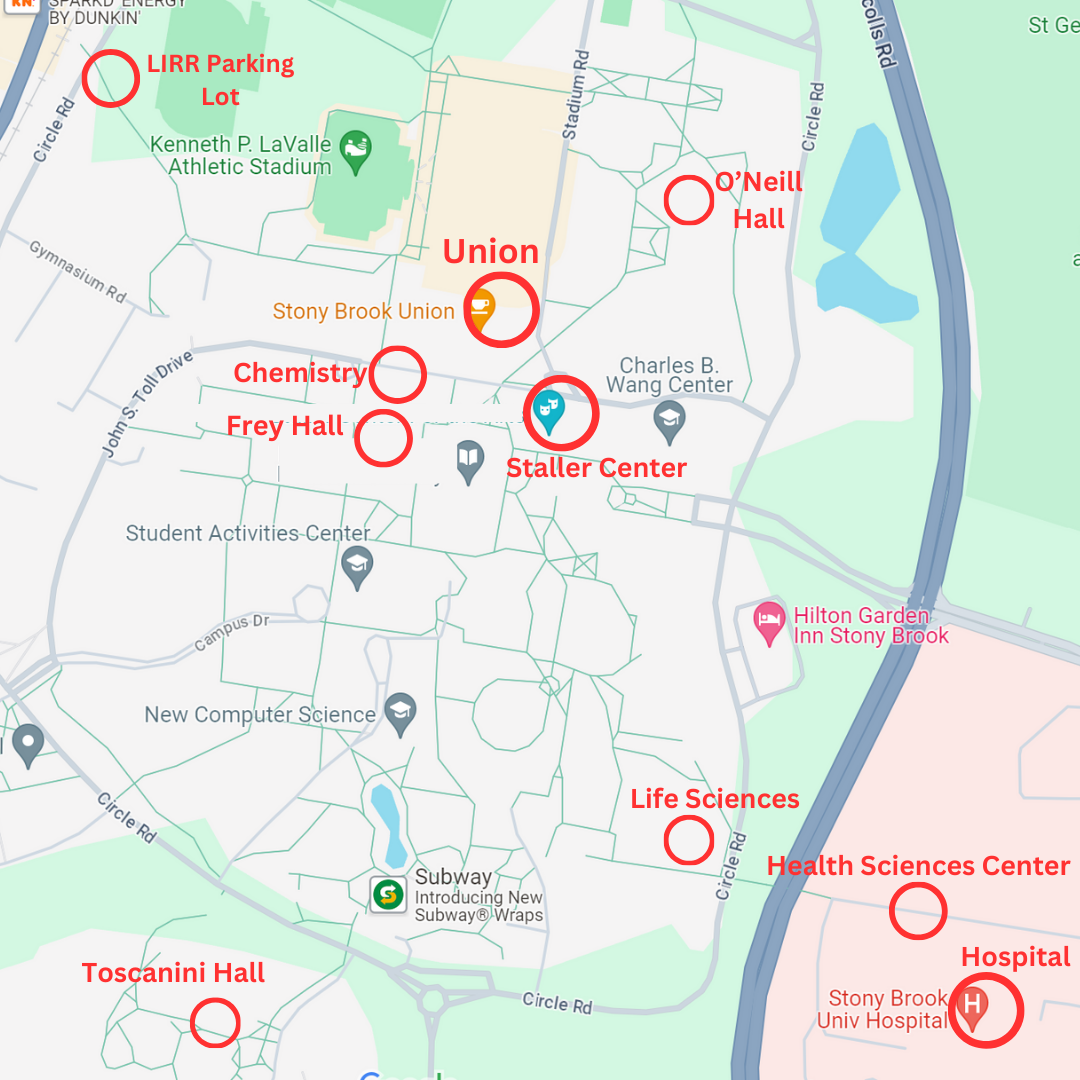
He then brainstormed with his team to develop a method that would take advantage of this difference in HDAC enzymatic activity. Ueki knew that the commercially available substrate bound well to HDAC. Using this structure, and through collaborations with the chemistry department at Stony Brook University, they were able to develop a prodrug strategy for drug delivery.
Imagine the drug to be a sphere that is connected by a string or bond to three other balls that are strung together. In total, there is a complex of four spheres. The drug is initially inactive and stays bound to the complex. When the complex encounters HDAC, which is expressed differentially in cancer cells, the HDAC enzyme cuts the string between the two balls at the end, leaving behind the drug connected to two balls. At this point, in a lab experiment, a harsh protease treatment—like scissors that cut up proteins, they are enzymes used to cut off remaining molecules on the drug—using trypsin would be used to cut off the last two spheres connected to the drug. However, the procedure using cell disruption and trypsin treatment in the body would not be feasible.
Ueki and his team then began a second search for an enzyme that would cut the string connecting the drug and the two spheres and which was differentially expressed in cancer cells. They eventually landed upon a protease called cathepsin L (CTSL) that is found in cancer cells and can cleave the string or bond without disrupting the cell.
Therefore, the starting material of a drug plus three-molecule complex is reduced to only the drug through the use of HDAC and CTSL, which cut off the other molecules.
Overall, Ueki’s method transforms a previously inactive drug into an active drug through conditions only found in cancer cells. Thus, the drug will only be activated in cancer cells and will stay inactive in normal cells.
So far, this novel drug delivery system has been tested in animal models with high efficiency. Once the drug is administered using this method, tumors stopped growing and even reduced in size.
“If this drug was administered normally, it is so powerful that all cells, cancerous and normal, would have died in two to three days,” Ueki explained. With this technique, he said, “only the cancer cells died…normal cells did not die and continued to grow.”
Ueki and his team are currently investigating ways to further improve the delivery system to make it faster and more effective. They hope to continue animal studies and eventually test the drug delivery system in humans.
This system can also be used in the future to deliver other drugs to cancer cells. Ultimately, Ueki hopes that his work “helps people and leads to the better treatment of cancer patients.”