Dr. Carl Tack is revolutionizing treatment of cancerous tumors in the liver as one of the only radiologists in the nation to use an innovative new procedure.
The liver is prone to tumors that originate from liver cancer or tumors that spread there from colon, breast, or other cancers.
Tack explained that over 50 percent of patients with these tumors die of liver failure, creating a need to prolong the lives of patients.
To do this, Tack combines two new technologies, LC beads and the surefire infusion system. LC beads are beads about 70 to 100 microns in size that are coated with chemotherapeutic agents.
The tiny size of these newly utilized beads increases treatment effectiveness by allowing drugs to reach deeper into the tumor. Once the drugs leave the drug-eluting bead, they go into the arterial blood of the liver and circulate for 14 days killing tumor cells.
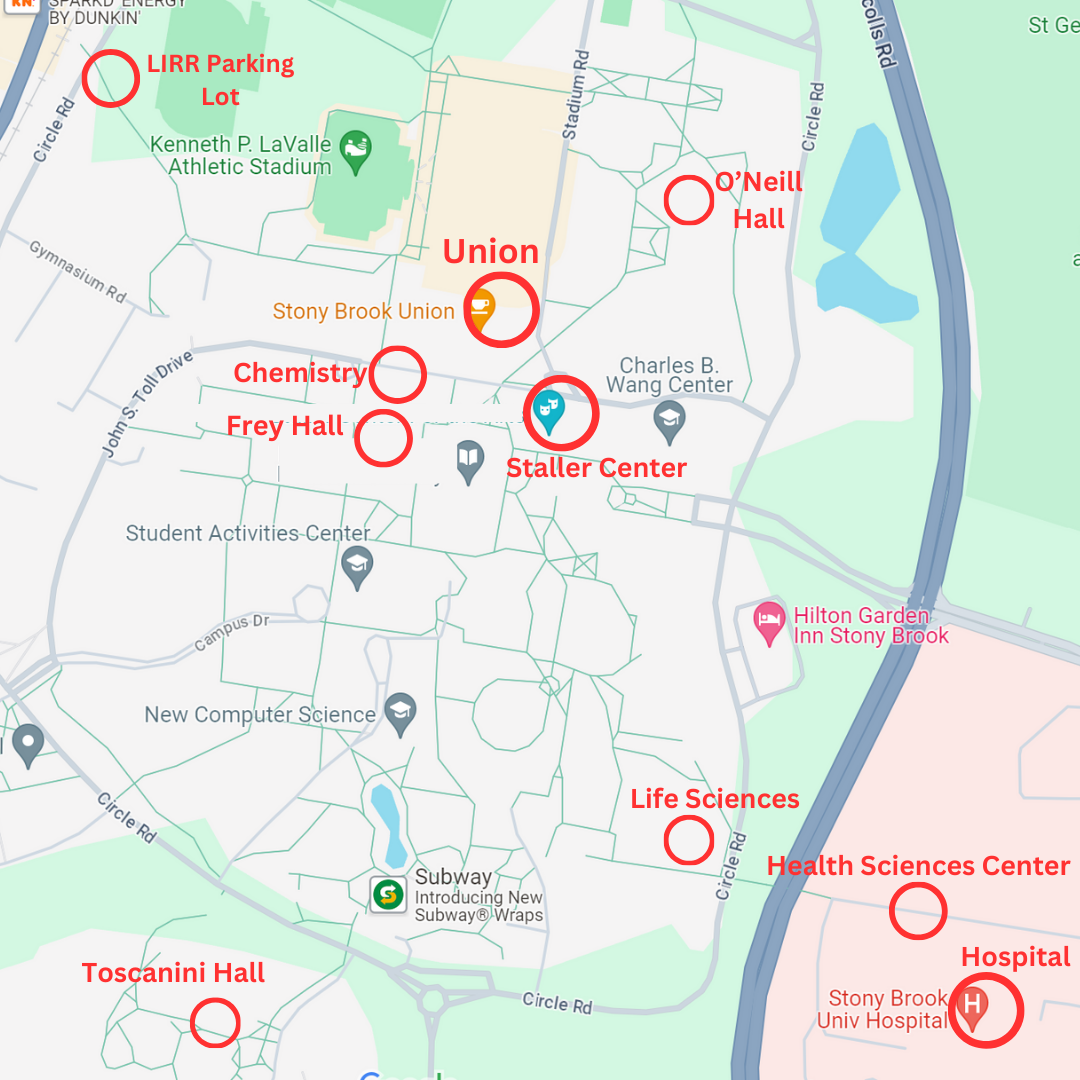
These beads are inserted into the body using the surefire infusion system, as Tack demonstrated using MRI and CT scans. The surefire infusion system, which has been used for six months, is a special catheter designed to prevent the reflux of beads and increase the number of beads that reach the target.
Tack is the first physician in New York State to use LC beads, the first to use the surefire system on Long Island and one of a few physicians in the country to put both technologies together.
The release of LC beads through the surefire system is effective because the surefire system increases pressure in the artery and collateral vessels in the area of the tumor open up.
Then, the beads are released and block the vessels, thereby blocking blood flow to the tumor.
This kills the tumor by both starving the tumor cells of oxygen and nutrients, and by stopping their replication through the use of chemotherapy drugs on the beads.
Tack observed that this treatment “is over six times more effective than previous treatment options.” Intravenous chemotherapy, a widely used treatment option for most cancers, involves chemotherapeutic drugs that are circulated throughout the entire body, therefore leading to varied and painful side effects.
The use of the catheter system is more selective and effective because it directly targets tumor cells, resulting in fewer side effects.
This treatment option is most effective for small recurring tumors or tumors that cannot be removed from surgery, which comprise 75 percent of liver tumor cases.
Patients with late stage cancer or patients with medical conditions like cirrhosis that make surgery dangerous, are those highly considered for the procedure, because while it is very effective, the treatment is powerful and can lead to liver failure.
“Titrating the power of the therapy,” Tack said, is the key to success.
Tack has been able to do just that. He spoke of a male patient in his 40s, whose name was not disclosed for medical privacy, who was given a prognosis of three months to live due to bowel cancer that had metastasized to the liver.
Through the use of the LC beads combined with the surefire system, Tack and his team have prolonged the patient’s life for over two years.
Although many have already benefitted from this treatment, Tack emphasized the need for increased awareness as he said, “most people just don’t know about it.”
Awareness of treatment options like the surefire infusion system will only become more vital as “increasing cases of Hepatitis B and C are likely to cause an increase in the prevalence of liver cancer,” Tack said.
He believes this procedure will become common in the future and hopes that increased awareness and use of this treatment will continue to combat cancerous liver tumors and prolong the lives of patients.